Does insurance cover scoliosis surgery? Navigating the complexities of medical insurance can feel daunting, especially when facing a potentially costly procedure like scoliosis surgery. This comprehensive guide unravels the intricate factors influencing insurance coverage decisions, empowering you to understand your options and plan effectively. From the various types of scoliosis surgery and pre-surgical considerations to the post-operative recovery process and insurance claim procedures, we’ll provide a clear and concise overview of the critical aspects surrounding this important question.
This guide will delve into the intricacies of coverage, exploring the nuanced perspectives of different insurance plans. We’ll compare HMOs and PPOs, analyze typical coverage percentages, and highlight the often-overlooked role of pre-authorization and documentation. By examining the pre-surgical evaluations, surgical procedures, and post-surgical recovery, you’ll gain a clearer picture of the total process and its financial implications.
Coverage Overview
Insurance, a crucial safety net for medical expenses, often covers a portion of medical procedures, including scoliosis surgery. Understanding the intricacies of insurance coverage is paramount for patients navigating the financial aspects of such a significant medical intervention. The specifics of coverage, however, are often nuanced and depend on numerous factors, influencing the overall cost burden.Insurance companies assess the cost and necessity of a medical procedure, weighing it against the potential risk and long-term implications.
This assessment, combined with the patient’s specific policy, dictates the extent of coverage. A thorough understanding of these factors can empower patients to proactively manage the financial aspects of their scoliosis treatment.
Factors Influencing Insurance Decisions
Insurance companies employ a multi-faceted approach to determine coverage for scoliosis surgery. Medical necessity, the severity of the condition, and the proposed treatment plan all play crucial roles in the insurance company’s decision-making process. The surgeon’s qualifications and experience, the hospital’s reputation, and the specific surgical techniques used also contribute to the evaluation. The company will also scrutinize the potential long-term implications of the procedure and the patient’s overall health history.
These factors are all considered before a final determination of coverage is made.
Common Exclusions and Limitations
Insurance policies often contain exclusions and limitations regarding spinal surgeries. Pre-existing conditions, particularly if not disclosed or managed appropriately, can lead to reduced coverage or outright denial. Furthermore, the policy’s definition of “medically necessary” plays a significant role, and procedures deemed elective or not essential may not be covered. The extent of the surgery and the associated complications also influence the coverage.
For instance, a more complex, high-risk surgery with a longer recovery period might face greater scrutiny and potential limitations.
While insurance coverage for scoliosis surgery varies significantly, understanding the specifics of your policy is crucial. Factors like pre-existing conditions and the surgeon’s qualifications often play a role. This is in contrast to the legal minimum age to rent a house, which is often determined by state and local regulations, as well as the specifics of the lease agreement.
Minimum age to rent a house requirements can differ greatly from state to state, impacting renters. Ultimately, securing coverage for scoliosis surgery hinges on detailed policy review and potentially, a consultation with an insurance professional.
Comparison of Insurance Plan Types
Different types of insurance plans, such as Health Maintenance Organizations (HMOs) and Preferred Provider Organizations (PPOs), have distinct approaches to scoliosis surgery coverage. HMOs typically require referrals from a primary care physician and often limit the choice of surgeons. PPOs, on the other hand, offer greater flexibility in choosing providers and often have broader networks of participating surgeons.
The specific terms and conditions, including co-pays, deductibles, and out-of-pocket maximums, will vary depending on the plan. The choice of plan type, therefore, can significantly impact the patient’s financial responsibility.
Typical Insurance Coverage Percentages
| Insurance Plan Type | Typical Coverage Percentage (Approximate) |
|---|---|
| HMO | 60-80% |
| PPO | 70-90% |
| Medicare | Varying, often lower for non-essential procedures |
| Medicaid | Varying, often based on state guidelines |
Note: These percentages are approximate and can vary significantly based on individual policy details, specific surgical procedures, and other factors. Coverage percentages can be lower or higher depending on the specific circumstances.
Scoliosis Surgery Types
Scoliosis, a spinal curvature disorder, can significantly impact a person’s quality of life. Fortunately, various surgical interventions are available to address the condition and restore spinal alignment. These procedures, meticulously tailored to individual needs, aim to prevent further progression of the curvature and alleviate associated symptoms. Understanding the diverse approaches is crucial for informed decision-making.The selection of a scoliosis surgical procedure depends on several factors, including the severity of the curvature, the patient’s age, and the location of the spinal curve.
Experienced orthopedic surgeons carefully evaluate these factors to determine the most suitable intervention. This evaluation often involves sophisticated imaging techniques and a comprehensive analysis of the patient’s medical history.
Surgical Procedures for Scoliosis Correction
Different types of scoliosis surgeries cater to varying degrees of curvature and spinal involvement. These procedures are designed to correct the deformity, stabilize the spine, and potentially improve breathing and overall well-being.
- Posterior Spinal Fusion: This procedure involves accessing the spine from the back (posterior). Surgeons create a stable structure by connecting the vertebrae using bone grafts and screws. This fusion aims to eliminate motion between the affected vertebrae, preventing further curvature. Pre-operative evaluations often include assessing the patient’s overall health and identifying any potential complications. Post-operative care involves pain management, physical therapy, and monitoring for complications such as infection or nerve damage.
This procedure is commonly used for moderate to severe scoliosis cases. For example, a patient with a 40-degree curvature might benefit from this approach.
- Anterior Spinal Fusion: This approach involves accessing the spine from the front (anterior). Surgeons address the deformity by fusing the vertebrae, often employing bone grafts and other supportive devices. Pre-operative considerations include evaluating the potential impact on adjacent structures and assessing the patient’s ability to tolerate the surgery. Post-operative care emphasizes monitoring for bleeding, infection, and nerve damage. Anterior fusion is typically employed for curves located in the thoracic or lumbar spine.
For example, a patient with a significant curvature impacting their breathing could benefit from this procedure.
- Combined Anterior-Posterior Spinal Fusion: This approach combines both anterior and posterior procedures to address complex scoliosis cases. The anterior approach often targets the front of the spine, while the posterior approach stabilizes the back. This combined approach offers comprehensive correction and stability. Pre-operative assessments focus on the complexity of the spinal curvature and potential complications. Post-operative care is often more intensive, involving careful monitoring for complications specific to both anterior and posterior approaches.
This is suitable for patients with severe curves involving multiple spinal segments. For instance, a patient with a large curvature spanning several vertebrae may require this technique.
Surgical Techniques
A variety of surgical techniques are used to achieve scoliosis correction. These techniques often involve the use of specialized instrumentation and bone grafting materials.
- Instrumentation: The use of rods, hooks, screws, and other implants provides structural support during the healing process. This allows for gradual correction of the spinal curve. Different types of instrumentation are chosen based on the individual’s specific needs. For example, some techniques utilize specialized screws to better target the curvature and provide a more stable correction.
- Bone Grafts: Bone grafts stimulate fusion by providing a framework for new bone growth, effectively creating a solid connection between the vertebrae. The choice of bone graft material is often guided by factors such as the patient’s age, the location of the curve, and the overall health of the spine. For example, autogenous grafts, derived from the patient’s own bone, are commonly employed.
Potential Complications
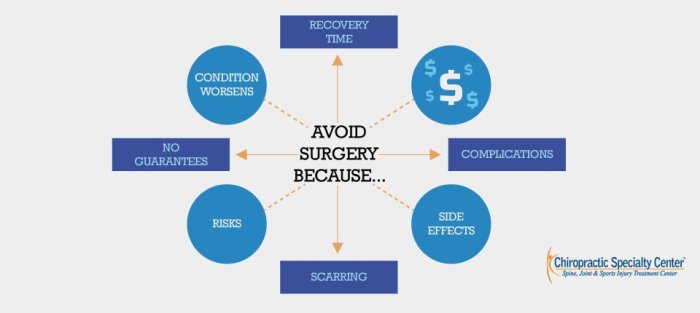
While scoliosis surgery is generally safe, potential complications can arise. Careful planning and meticulous execution of the procedure are essential to minimize these risks.
- Nerve Damage: Injury to the spinal nerves is a possible complication, requiring close monitoring during and after the procedure. Surgeons carefully navigate around the delicate nerves to minimize this risk.
- Infection: Infection at the surgical site is a concern, necessitating appropriate antibiotic protocols and diligent post-operative care. Strict adherence to infection prevention protocols is crucial to minimize the risk.
- Bleeding: Excessive bleeding can be a complication, requiring blood transfusions or other interventions. Surgeons take steps to minimize blood loss and address it promptly if it occurs.
Scoliosis Surgery Overview Table
| Surgery Type | Typical Duration (hours) | Recovery Time (weeks/months) |
|---|---|---|
| Posterior Spinal Fusion | 3-6 | 6-12 weeks |
| Anterior Spinal Fusion | 4-8 | 8-16 weeks |
| Combined Anterior-Posterior Fusion | 6-10 | 10-18 weeks |
Pre-Surgical Considerations
Navigating the intricate landscape of scoliosis surgery often requires a thorough understanding of pre-surgical evaluations. These crucial steps pave the way for informed decisions, ensuring the procedure aligns with the patient’s specific needs and maximizes the chances of a successful outcome. Understanding the pre-surgical process is paramount for both patients and insurance providers to ensure the procedure is both medically necessary and financially feasible.The pre-surgical phase involves a comprehensive assessment, aiming to meticulously determine the appropriateness of the surgical intervention.
This assessment includes not only physical examinations but also diagnostic tests to precisely define the scoliosis’s severity, progression, and overall impact on the patient’s well-being. A clear understanding of the patient’s medical history, coupled with detailed imaging results, enables healthcare professionals to make well-informed decisions about the necessity and feasibility of the surgery. These considerations are essential for a smooth and successful surgical journey.
Pre-Surgical Evaluations and Diagnostic Tests
Pre-surgical evaluations are pivotal in determining the suitability of scoliosis surgery. These evaluations meticulously assess the patient’s overall health, the extent of the spinal deformity, and potential risks. Comprehensive evaluations involve a detailed medical history, physical examination, and a series of diagnostic tests. These tests are crucial in providing a comprehensive picture of the patient’s condition and guiding treatment decisions.
Factors Affecting Insurance Coverage Decisions
Several factors influence insurance coverage decisions during pre-surgical evaluations. These factors include the severity of the scoliosis, the potential risks associated with surgery, the patient’s overall health, and the specific type of surgical procedure being considered. The documentation provided by the medical professionals plays a critical role in convincing insurance companies of the necessity and appropriateness of the surgical intervention.
- Severity of the Scoliosis: The degree of spinal curvature significantly impacts the decision-making process. Insurance companies often require evidence of a substantial and progressive curvature that necessitates surgical intervention. Mild cases may not qualify for coverage.
- Patient’s Overall Health: Pre-existing medical conditions and overall health status are crucial factors. A patient with significant comorbidities may have their coverage limited, especially if these conditions are considered to increase surgical risks.
- Surgical Risk Assessment: The potential risks and complications of surgery are carefully considered. A detailed risk assessment, conducted by medical professionals, is essential in determining if the surgical benefits outweigh the potential risks for the individual patient.
- Surgical Procedure: The specific type of surgical procedure and its suitability for the patient’s condition significantly influence coverage decisions. Insurance companies might favor less invasive options whenever feasible.
Role of Medical Professionals in Determining Surgical Need
Medical professionals, including orthopedists, neurosurgeons, and other relevant specialists, play a critical role in evaluating the need for scoliosis surgery. They conduct thorough examinations, interpret diagnostic test results, and provide a comprehensive assessment of the patient’s condition. The documentation provided by these specialists is crucial for convincing insurance companies of the necessity of the surgical intervention. This documentation includes medical reports, imaging results, and detailed explanations of the surgical plan.
Common Documentation Required by Insurance Companies
Insurance companies typically require specific documentation before approving scoliosis surgery. This documentation helps them assess the necessity of the procedure and ensure that it aligns with their coverage policies.
- Medical History: A detailed medical history, including previous diagnoses, treatments, and any relevant family history, is often required.
- Imaging Studies: X-rays, CT scans, and MRI scans are frequently needed to assess the severity and extent of the scoliosis.
- Surgical Report: A detailed surgical plan, outlining the proposed procedure, expected outcomes, and potential risks, is vital.
- Physician’s Certification: A physician’s statement justifying the necessity of the surgery based on the patient’s specific condition is a critical component.
Typical Pre-Surgical Tests and Their Importance
The table below Artikels common pre-surgical tests and their significance in determining insurance coverage. These tests help paint a comprehensive picture of the patient’s condition and aid in the assessment of the necessity of surgical intervention.
| Test | Importance in Determining Coverage |
|---|---|
| X-rays | Provides initial assessment of spinal curvature and deformity, crucial for initial diagnosis and coverage evaluation. |
| CT Scan | Offers detailed cross-sectional views, enabling a more precise evaluation of the spinal structure and its surrounding tissues. This is critical for assessing complex deformities. |
| MRI Scan | Offers detailed soft tissue imaging, important for evaluating nerve root involvement and other soft tissue structures. Essential for ensuring a comprehensive assessment before surgery. |
| Blood Tests | Evaluates overall health and identifies any underlying conditions that might influence surgical risk. Helps ensure the patient is in good enough health for surgery. |
| Pulmonary Function Tests | Assesses lung capacity and function, particularly important in patients with severe scoliosis, where the curvature may impact breathing. This is a crucial factor in the assessment of surgical risk. |
Post-Surgical Recovery
The road to recovery after scoliosis surgery is a journey, not a sprint. Patients can expect a period of healing and adjustment, marked by varying levels of pain and restrictions. Understanding the stages of recovery, potential complications, and the importance of diligent follow-up care is crucial for a successful outcome. A proactive approach, combined with a supportive medical team, will pave the way for long-term well-being.
Typical Post-Operative Recovery Period
The post-operative recovery period following scoliosis surgery is typically characterized by several phases. Initial days are focused on pain management and stabilization. Weeks and months afterward, patients progressively regain strength and mobility, with a gradual return to daily activities. The duration and specifics of this recovery period are highly individualized, depending on the severity of the curvature, the surgical approach, and the patient’s overall health.
Potential Complications During Recovery
While scoliosis surgery is generally safe and effective, potential complications can arise during the recovery process. These may include infection at the surgical site, blood clots, or nerve damage. Proper wound care, vigilant monitoring, and prompt medical intervention are essential to address these issues. Post-operative pain management is critical, and careful adherence to prescribed medication regimens, as well as communication with the medical team, can mitigate potential complications.
While researching whether insurance covers scoliosis surgery, you might find yourself craving a breathtaking view. Cincinnati boasts some amazing rooftop restaurants, offering stunning cityscapes, and a perfect place to unwind while you ponder your insurance coverage options. Best rooftop restaurants in Cincinnati are a great way to reward yourself while you investigate your insurance options further.
Ultimately, the specifics of insurance coverage for scoliosis surgery vary greatly, and a thorough consultation with your provider is essential.
Long-Term Effects of Scoliosis Surgery
The long-term effects of scoliosis surgery are generally positive. Most patients experience a significant improvement in posture and spinal stability, leading to reduced back pain and improved quality of life. However, some patients may experience lingering discomfort or require further adjustments in the long term. This emphasizes the importance of ongoing monitoring and support to address any potential long-term issues.
Importance of Follow-Up Care and Rehabilitation
Regular follow-up appointments with the surgeon are critical to monitor the healing process and address any concerns. Rehabilitation plays a vital role in restoring strength, flexibility, and range of motion. Physical therapy exercises, tailored to the individual’s needs, can significantly accelerate recovery and improve long-term outcomes.
Stages of Recovery
| Stage | Expected Pain Level | Allowed Activities |
|---|---|---|
| Phase 1 (First 2-4 weeks) | High to Moderate | Limited activity, bed rest, pain management, wound care, light exercises as prescribed. |
| Phase 2 (4-8 weeks) | Moderate to Low | Gradual increase in activity, mobility exercises, light household chores, and short walks, as tolerated. |
| Phase 3 (8-12 weeks) | Low | Return to most daily activities, but avoiding strenuous activities. May return to school or work with limitations. |
| Phase 4 (Beyond 12 weeks) | Minimal | Full range of activities, return to normal routine, with ongoing monitoring and follow-up care. |
Insurance Claim Process
Navigating the insurance claim process for scoliosis surgery can feel daunting. Understanding the steps involved, timelines, and necessary documentation empowers patients and families to effectively manage the financial aspects of this significant procedure. This section will detail the process, emphasizing clarity and actionable information.
Claim Filing Steps
The insurance claim process typically begins with pre-authorization, a critical step to ensure coverage. This involves submitting medical records, the surgeon’s proposal, and potentially an estimate of the total cost. Insurance companies may request additional information, like a detailed description of the surgical approach, pre-operative evaluations, and post-operative expectations. These steps ensure the insurance company understands the specifics of the case and can assess coverage.
Timeframe for Approval and Payment
The timeframe for insurance approval and payment varies significantly depending on the insurance company, the complexity of the case, and the thoroughness of the submitted documentation. Some insurance companies may have a quicker turnaround time for simpler cases, while more intricate ones could take several weeks or even months. Factors like prior authorizations, appeals, and the availability of necessary medical reports all contribute to the total duration.
For instance, a straightforward case might be approved within 2 weeks, whereas a case requiring complex pre-authorization and multiple revisions could take 6-8 weeks.
Required Documentation, Does insurance cover scoliosis surgery
Comprehensive documentation is crucial for a successful claim. This typically includes pre-operative reports, including medical history, diagnostic imaging results (X-rays, CT scans, MRIs), and the surgeon’s detailed treatment plan. Post-operative reports and follow-up records, including discharge summaries, prescriptions, and rehabilitation plans, are also vital. The specific documentation requirements vary depending on the insurance provider, so it’s imperative to consult your policy and the insurance company’s guidelines.
Always retain copies of all submitted documents.
Potential Reasons for Claim Denial and Addressing Them
Insurance claims can be denied for various reasons, including lack of pre-authorization, inadequate documentation, or discrepancies in the surgical procedure compared to the approved plan. If a claim is denied, it’s important to understand the reasons. Review the denial letter carefully and gather any missing documentation. Contact the insurance company to discuss the denial and inquire about the required steps to appeal the decision.
Seeking guidance from a medical billing specialist or an insurance advocate can be invaluable in these situations. The denial letter will usually Artikel the reasons for the denial, which provides a clear path for appeal.
Claim Process Overview
| Step | Timeline | Necessary Documents |
|---|---|---|
| Pre-authorization Request | 1-2 weeks | Medical records, surgeon’s proposal, cost estimate |
| Insurance Approval | 1-8 weeks (variable) | Complete medical records, diagnostic reports, treatment plan |
| Claim Submission | Upon approval | All approved documentation, receipts, and bills |
| Payment Processing | 1-4 weeks (variable) | All supporting documents |
| Follow-up and Appeals (if needed) | Variable | Denial letter, supporting documentation |
Specific Insurance Policies: Does Insurance Cover Scoliosis Surgery
Navigating the labyrinth of insurance coverage for scoliosis surgery can feel daunting. Understanding the specifics of your policy is crucial, as the details often dictate the financial burden of this procedure. Different plans have varying approaches to coverage, impacting the out-of-pocket expenses for patients. This section delves into the specifics, examining how different policy types handle pre-authorization, deductibles, and other crucial factors.
Policy Variations in Coverage
Insurance policies, like individuals, are diverse. A single policy can differ significantly from another. This variance often stems from factors such as the type of plan (e.g., HMO, PPO, EPO), the insurer’s specific provisions, and the plan’s financial resources. These factors influence how the insurance company views and handles the necessity and costs of scoliosis surgery.
Deductibles, Co-pays, and Coinsurance
These three terms are crucial to understanding your out-of-pocket expenses. Deductibles represent the amount you must pay before your insurance begins covering the cost of the surgery. Co-pays are fixed fees you pay for specific services, such as a doctor’s visit or surgery. Coinsurance is a percentage of the cost of a service that you are responsible for paying.
For instance, a 20% coinsurance rate means you pay 20% of the medical bill after the deductible is met. These components, in combination, often determine the financial impact of the surgery. For example, a high deductible plan might mean you bear a significant upfront cost before insurance kicks in.
Pre-authorization Requirements
Pre-authorization is a process where your insurance company reviews the necessity and appropriateness of a medical procedure. This is a common practice to manage healthcare costs and ensure that the proposed treatment is medically necessary and aligns with established standards of care. Some policies may require pre-authorization for scoliosis surgery, requiring documentation of the diagnosis, surgical plan, and the surgeon’s qualifications.
Failure to obtain pre-authorization can lead to denial of claims. The exact pre-authorization process can differ considerably between insurers.
Comparison of Coverage Across Policy Types
| Policy Type | Deductible | Co-pay | Coinsurance | Pre-authorization Requirements |
|---|---|---|---|---|
| HMO (Health Maintenance Organization) | Typically lower or higher than PPO, depending on the plan | Usually lower than PPO | Potentially higher than PPO | Generally stricter and require pre-authorization |
| PPO (Preferred Provider Organization) | Typically higher than HMO | Usually higher than HMO | Potentially lower than HMO | Generally less strict and allow greater flexibility in choosing providers |
| EPO (Exclusive Provider Organization) | Can vary | Usually lower than PPO, higher than HMO | Potentially lower than HMO | Generally less strict than HMO but require pre-authorization |
This table provides a general overview. Specific details can vary greatly between individual plans. Always refer to your policy documents for precise information.
Understanding Policy Language
Insurance policies are often dense with legal jargon. Pay close attention to clauses that specify coverage for pre-existing conditions, the scope of procedures covered, and the conditions under which coverage may be denied. It is often advisable to consult with a qualified insurance professional to ensure a comprehensive understanding of your policy’s stipulations regarding scoliosis surgery. Furthermore, reviewing the specific details of the plan can help determine if the plan covers the surgery or if additional costs may apply.
Appealing Denied Claims
A denied insurance claim for scoliosis surgery can feel like a significant setback, leaving patients and families grappling with uncertainty and financial burdens. However, the process of appealing a denied claim is often a crucial step in achieving the necessary care. Understanding the process, your rights, and how to build a strong appeal is paramount. This guide provides a roadmap to navigate this complex situation.Insurance companies have established procedures for claims denials, often citing specific criteria for coverage.
This necessitates a meticulous approach to understanding the reasons behind the denial and the steps required to successfully appeal. A well-prepared appeal, supported by comprehensive documentation, significantly increases the likelihood of favorable results.
Understanding Denial Reasons
Insurance companies often deny claims for scoliosis surgery due to various factors. These can range from questions about the necessity of the surgery, the surgeon’s qualifications, or whether the proposed treatment aligns with their pre-defined coverage guidelines. The specific reason for denial is crucial for crafting a targeted appeal. Thorough examination of the denial letter and supporting documentation is essential.
This includes a clear understanding of the specific criteria the insurance company used to deny the claim. This helps in understanding the weak points in the initial claim and how to strengthen the appeal.
Patient Rights in Appeal Process
Patients have specific rights during the appeal process. These rights typically include access to the reasons for denial, the opportunity to provide additional information or documentation, and a clear timeline for the review process. Understanding these rights empowers patients to proactively engage with the insurance company and ensure they are treated fairly. Patients should actively seek clarity on the specific appeals process Artikeld in their insurance policy.
This proactive approach can avoid potential delays and ensure the appeal process unfolds smoothly.
Steps to Appeal a Denied Claim
Appealing a denied claim requires a systematic approach. A step-by-step guide will assist in this process.
- Review the Denial Letter Carefully: Carefully scrutinize the denial letter for specific reasons for denial. Note any references to policy provisions, medical necessity guidelines, or other criteria used to deny coverage. This is the foundation of your appeal strategy. Identifying the specific points of contention allows you to address them directly and effectively.
- Gather Supporting Documentation: Collect all relevant medical records, including physician reports, diagnostic imaging results, and any other documentation supporting the need for surgery. Ensure all supporting documents are organized chronologically and clearly labeled for ease of reference. Detailed records help strengthen your appeal.
- Consult with Legal Counsel (Optional): In complex cases or when the denial is significant, seeking advice from an attorney specializing in insurance claims can be beneficial. Legal counsel can provide guidance on navigating the legal aspects of the appeal process and ensure your rights are protected.
- Prepare a Compelling Appeal Letter: Draft a well-structured letter outlining the reasons for appeal, addressing the specific points of contention in the denial letter, and providing additional supporting evidence. Be concise, clear, and factual in your appeal letter. Maintain a professional tone and avoid emotional language.
- Submit the Appeal Letter and Supporting Documents: Submit the appeal letter and all supporting documentation to the insurance company using the designated appeal process Artikeld in their policy. Maintain records of submission and follow up as needed.
- Follow Up and Monitor the Process: Regularly check the status of your appeal with the insurance company. This demonstrates your commitment to the process and ensures you are informed of any necessary next steps. Maintain communication to keep the appeal process moving forward.
Examples of Successful Appeals and Common Reasons for Denial
Numerous successful appeals have been achieved by highlighting the medical necessity of the surgery, providing comprehensive documentation, and effectively addressing the specific concerns raised by the insurance company. A common reason for denial is the perceived lack of medical necessity. Other factors include limitations on surgeon qualifications, the perceived suitability of alternative treatments, and issues with pre-authorization or claim submission procedures.
Importance of Maintaining Thorough Records
Thorough documentation is crucial throughout the entire process. Maintaining a comprehensive record of all communications, medical reports, and supporting documentation ensures a strong foundation for the appeal. This comprehensive approach will aid in demonstrating the need for surgery and addressing any concerns the insurance company may have.
Preparing a Compelling Appeal Letter
A compelling appeal letter is a key component of the appeal process. The letter should clearly state the reason for the appeal, clearly articulate the specific points of contention, and provide concise supporting evidence. The letter should be well-organized, concise, and professional. Each section of the letter should be clearly presented, enhancing readability and providing clarity to the insurance company.
Preventive Measures
A whispered promise of a life free from the scalpel’s touch, a life where the spine stands tall and straight, is within reach for many with scoliosis. Preventive measures play a crucial role in this journey, offering a path toward a healthier spine and minimizing the need for potentially invasive surgical interventions. Early detection and proactive management can often significantly alter the course of scoliosis, potentially preventing it from progressing to a stage requiring surgery.Understanding the nuances of scoliosis prevention requires a comprehensive approach encompassing early identification, non-surgical treatments, and proactive lifestyle choices.
The journey towards a scoliotic-free future begins with knowledge and the commitment to taking preventative steps.
Early Detection and Intervention
Early detection of scoliosis is paramount in its management. The sooner the condition is identified, the more effective and less invasive the treatment options become. Regular check-ups, especially during crucial growth spurts, are vital. Pediatricians and orthopedists are well-equipped to detect subtle spinal deviations through visual assessments and specialized imaging techniques. Prompt intervention can halt or significantly slow the progression of the curve, potentially preventing the need for surgical correction.
Non-Surgical Treatment Options
Non-surgical treatments are often the initial line of defense against the progression of scoliosis. These methods aim to reduce pain, improve posture, and maintain spinal health. They are particularly effective in managing mild to moderate scoliosis cases. Bracing is a common non-surgical intervention. Specialized braces, tailored to the individual’s spinal curve, can help control the progression of the curve.
Role of Physical Therapy and Other Conservative Treatments
Physical therapy plays a vital role in managing scoliosis, especially when combined with bracing or other conservative treatments. Exercises designed to strengthen core muscles, improve posture, and increase spinal flexibility can be highly effective in slowing the progression of the condition. These exercises, often guided by a physical therapist, are tailored to the specific needs of each patient.
Other conservative treatments might include lifestyle modifications, such as maintaining a healthy weight, practicing good posture, and avoiding activities that exacerbate spinal pain.
Potential Preventive Measures and Their Effectiveness
- Regular check-ups: Crucial for early detection. Early identification significantly increases the chance of successful non-surgical management.
- Proper posture: Maintaining good posture throughout the day can help prevent the development and progression of scoliosis. This includes using good posture at desks, while working, and while playing.
- Healthy weight management: Maintaining a healthy weight can reduce the strain on the spine, thereby potentially reducing the risk of scoliosis. Excess weight can contribute to spinal stress and potential curve progression.
- Strengthening core muscles: Core strengthening exercises can enhance spinal stability and support. A strong core provides support and helps maintain proper posture, which can help slow the progression of scoliosis.
- Avoiding activities that strain the spine: Participating in activities that put excessive stress on the spine should be monitored. Excessive or repetitive strain can contribute to spinal curve progression.
- Proper nutrition: A balanced diet rich in essential nutrients is vital for overall health and bone development. Good nutrition contributes to healthy growth and can indirectly support spinal health.
Summary
In conclusion, understanding insurance coverage for scoliosis surgery involves a multifaceted approach. The decision hinges on factors ranging from the type of surgery to the specific provisions of your insurance policy. Thorough research, meticulous documentation, and a clear understanding of the pre- and post-operative stages are crucial. This guide aims to equip you with the knowledge needed to confidently navigate the process and make informed decisions about your care.
Remember, seeking professional advice from both your healthcare provider and insurance representative is paramount to ensuring a smooth and successful outcome.
FAQ
Does insurance cover the cost of all types of scoliosis surgery?
No, insurance coverage for scoliosis surgery varies significantly depending on the specifics of the procedure, the patient’s individual circumstances, and the terms of the insurance policy. Some procedures may be fully covered, while others may have partial or no coverage.
What factors affect the decision of insurance companies regarding coverage?
Insurance companies consider factors like the necessity of the surgery, the severity of the scoliosis, the surgeon’s credentials, and the pre-surgical evaluations. They also scrutinize pre-existing conditions and the potential complications of the surgery.
How long does the insurance claim process typically take?
The timeframe for insurance approval and payment can vary significantly. Factors such as the complexity of the claim, pre-authorization requirements, and the specific insurance provider all play a role.
What are some common reasons for a claim denial?
Common reasons for claim denial include inadequate documentation, lack of pre-authorization, misdiagnosis, or a determination that the surgery is not medically necessary. Understanding these potential issues is crucial for avoiding delays and potentially appealing a denial.
