Icd-10 code for stool occult blood screening medicare – Understanding the ICD-10 code for stool occult blood screening under Medicare is crucial for accurate billing and reimbursement. This process, vital for early detection of potential health issues, involves a specific code to document the screening, its result (positive or negative), and the subsequent Medicare coverage. This comprehensive guide details the code, its clinical context, Medicare coverage, and essential documentation requirements, empowering healthcare providers with the knowledge needed to navigate this critical process effectively.
Stool occult blood screening is a valuable diagnostic tool used to detect hidden blood in the stool. Early detection can significantly impact patient outcomes. The process typically involves a simple sample collection and laboratory analysis. Understanding the nuances of the ICD-10 code and Medicare reimbursement is vital to ensure accurate and timely processing of claims.
Introduction to Stool Occult Blood Screening
Stool occult blood screening is a crucial diagnostic tool for detecting hidden blood in the stool. It’s a non-invasive procedure that helps identify potential gastrointestinal issues, often serving as a primary screening step for conditions like colon cancer. This method is particularly valuable in early detection, as many gastrointestinal problems may not present obvious symptoms in their early stages.The screening process aims to identify even minute amounts of blood that aren’t visible to the naked eye.
It plays a vital role in the prevention and early treatment of diseases by allowing for prompt intervention. By identifying these subtle signs, healthcare providers can initiate investigations and potentially prevent more severe complications.
Screening Methods and Procedures, Icd-10 code for stool occult blood screening medicare
Accurate and timely results are critical in patient care. Delay in diagnosis can lead to worsening conditions and potentially poorer outcomes. Early detection enables prompt intervention, potentially saving lives and improving quality of life. This section details the different methods used for stool occult blood screening, highlighting the importance of accurate and timely results in patient care.
| Screening Method | Sample Type | Test Procedure | Typical Turnaround Time |
|---|---|---|---|
| Hemoccult | Stool sample | The sample is placed on a special card and a chemical reagent is applied. A color change indicates the presence of blood. | Usually within 24-48 hours. |
| Guaiac-based test | Stool sample | The stool sample is mixed with a chemical reagent. A positive test shows a color change, indicating the presence of blood. | Usually within 24-48 hours. |
| Immunochemical test | Stool sample | The stool sample is analyzed using antibodies that specifically target blood proteins. | Usually within 24-72 hours. |
Sample Collection and Testing
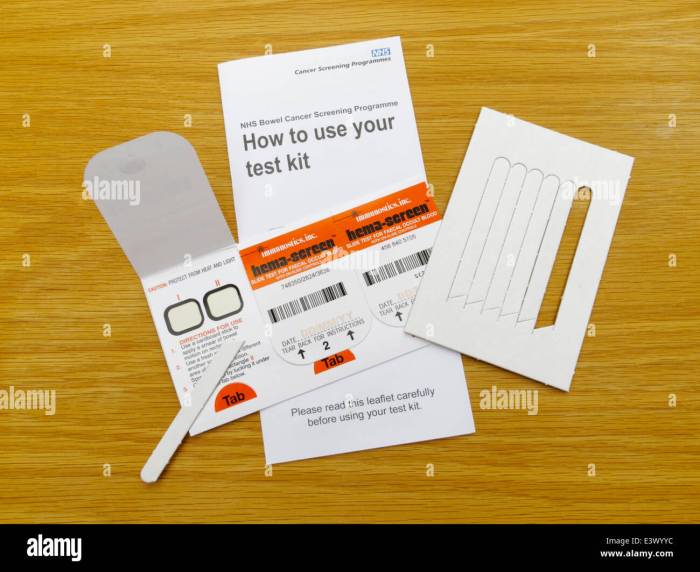
Collecting a stool sample for occult blood screening is a straightforward process. Patients are typically provided with collection kits, and instructions are given for proper sample handling and preservation to maintain the integrity of the sample for accurate testing. Strict adherence to these guidelines is essential for reliable results.
Importance of Accurate and Timely Results
Accurate and timely results are essential in managing patient care. A missed or delayed diagnosis can have severe consequences. Prompt intervention based on accurate results can significantly improve patient outcomes. For instance, early detection of colon cancer through stool occult blood screening allows for timely treatment, which can improve survival rates and overall quality of life.
ICD-10 Codes for Stool Occult Blood Screening
Stool occult blood screening is a crucial diagnostic tool for detecting hidden blood in the stool, often an indicator of potential gastrointestinal issues. Accurate coding of these results is vital for proper medical record-keeping and reimbursement. Understanding the associated ICD-10 codes is essential for healthcare professionals.The specific ICD-10 code used to document stool occult blood screening results depends largely on the outcome—positive or negative—and any associated clinical findings.
This information is critical for accurately reflecting the patient’s condition in the medical record. Further, accurate coding helps ensure appropriate billing and reimbursement for the screening procedure.
ICD-10 Code for Negative Results
Negative stool occult blood screening results indicate no detectable blood in the stool sample. This typically doesn’t necessitate a specific ICD-10 code, as the absence of the finding is implicitly documented by the test result. However, if a clinical evaluation is performed in conjunction with the screening, then a code related to that evaluation might be necessary.
ICD-10 Code for Positive Results
A positive stool occult blood screening result signifies the presence of hidden blood in the stool. The relevant ICD-10 code for this situation is usually tied to thesuspected* underlying condition or the associated symptoms. For instance, if the positive result is suspected to be due to a colorectal cancer or polyp, the corresponding ICD-10 code for the suspected diagnosis would be used, not the test itself.
Variations in Coding Based on Results
The coding approach can vary based on whether the result is positive or negative. A negative result, as previously discussed, doesn’t typically require a specific ICD-10 code for the test itself, but rather for the clinical evaluation if any. A positive result, however, necessitates a code reflecting the suspected underlying condition, if one is evident. If the underlying condition is not immediately apparent, a code for further investigation or a general code for gastrointestinal disorders might be used.
Table of ICD-10 Codes
| ICD-10 Code | Description | Clinical Context | Example Use Cases |
|---|---|---|---|
| K52.9 | Other specified disorders of the small intestine | Used when a positive occult blood result is found, but no specific cause is apparent. | A patient presents with positive stool occult blood, but further investigation is needed to determine the underlying cause. |
| K55.0 | Polyps of colon | Used when a positive occult blood test is found in conjunction with symptoms suggesting polyps. | Patient reports rectal bleeding and has a positive stool occult blood test. Colonoscopy reveals polyps. |
| C18.9 | Malignant neoplasm of colon | Used when a positive occult blood test is found and strongly suggests colorectal cancer. | Patient presents with abdominal pain, weight loss, and positive stool occult blood. Further investigation confirms colorectal cancer. |
| Z01.8 | Other screening procedures | Used if the screening itself is the primary focus. | Patient undergoing a routine checkup and having a stool occult blood test. |
Medicare Coverage and Reimbursement
Medicare’s coverage of stool occult blood screening is generally straightforward, but there are specific rules and guidelines to understand. Understanding these rules is crucial for both healthcare providers and patients to ensure appropriate billing and reimbursement. Knowing the criteria for coverage helps avoid potential issues down the line.
Medicare Coverage Policy
Medicare Part B covers certain preventive services, including stool occult blood testing. However, this coverage isn’t automatic. Specific conditions must be met for the screening to be covered. The key aspect is that it must be part of a preventive care plan. This aligns with Medicare’s focus on preventative health measures to maintain well-being.
Circumstances Under Which Medicare Covers Screening
Medicare covers stool occult blood screening when it’s part of a recommended preventive service schedule. This typically involves screening individuals at high risk for colorectal cancer, such as those aged 50 and older. It’s also relevant in instances where a patient has a family history of colorectal cancer or other relevant risk factors. The screening needs to be ordered and performed by a qualified healthcare professional within the scope of their practice.
Factors Influencing Reimbursement Amounts
Several factors can influence the reimbursement amount for stool occult blood screening. The most prominent factors are the specific type of screening test used, the facility where the test was performed, and the physician’s professional fees. Also, the presence of any complications during the procedure can also impact the amount paid. For example, if the test required a specialized procedure or additional staff time, the reimbursement may reflect these added costs.
Similarly, the complexity of the patient’s medical history can also be a factor.
Navigating the intricacies of the ICD-10 code for stool occult blood screening under Medicare can be complex. Fortunately, local resources like Longview State Bank Sidney IL might offer helpful information related to medical billing procedures, though a direct connection isn’t immediately apparent. Ultimately, understanding these codes remains crucial for accurate and efficient Medicare claims processing related to stool occult blood screening.
Table of Screening Types, Coverage, Reimbursement, and Documentation
| Screening Type | Medicare Coverage Criteria | Reimbursement Rate | Documentation Requirements |
|---|---|---|---|
| Fecal Immunochemical Test (FIT) | Covered for individuals aged 50 and older as part of routine colorectal cancer screening, and for those with a family history or other risk factors. The test needs to be ordered and performed by a qualified healthcare professional. | Reimbursement rates vary based on the specific facility, but generally fall within the range of Medicare’s fee schedule. Variations may be due to specific test kits, or lab processing fees. | Medical record should document the patient’s age, any relevant risk factors, the physician’s order, the date of the test, and the results. Any abnormal findings, as well as the physician’s interpretation of those results, must be documented. |
| Guaiac-based Fecal Occult Blood Test (FOBT) | Covered for individuals aged 50 and older as part of routine colorectal cancer screening, and for those with a family history or other risk factors. The test needs to be ordered and performed by a qualified healthcare professional. | Reimbursement rates vary based on the specific facility, but generally fall within the range of Medicare’s fee schedule. Variations may be due to specific test kits, or lab processing fees. | Medical record should document the patient’s age, any relevant risk factors, the physician’s order, the date of the test, and the results. Any abnormal findings, as well as the physician’s interpretation of those results, must be documented. |
Clinical Significance and Interpretation: Icd-10 Code For Stool Occult Blood Screening Medicare
A positive stool occult blood test result is a significant finding that warrants further investigation. It indicates the presence of blood in the stool, which could stem from a variety of sources, ranging from harmless conditions to serious diseases. Understanding the possible causes, the importance of follow-up, and the potential for errors is crucial for appropriate patient management.A positive result, while alarming, doesn’t automatically mean cancer.
Many benign conditions can cause occult blood in the stool, such as hemorrhoids, anal fissures, or inflammatory bowel disease. However, it also could be a sign of a more serious issue, like colorectal cancer. This highlights the critical need for careful evaluation and appropriate follow-up to determine the underlying cause.
Clinical Significance of a Positive Result
A positive stool occult blood test signifies the presence of hidden blood in the stool. This finding is clinically significant because it could indicate a range of conditions, from minor issues to life-threatening diseases. Prompt evaluation and appropriate follow-up are vital to accurately diagnose the cause and initiate appropriate treatment. The delay in addressing a potentially serious condition can have significant implications for patient outcomes.
Possible Causes of a Positive Result
A positive stool occult blood test result can stem from a variety of causes. These range from common, benign conditions to more serious, potentially malignant ones.
- Benign Conditions: These often involve issues in the lower digestive tract. Common examples include hemorrhoids (swollen veins in the anus), anal fissures (small tears in the lining of the anus), and inflammatory bowel disease (conditions that cause inflammation in the digestive tract). These conditions are usually treatable with appropriate medical interventions.
- Malignant Conditions: In some cases, a positive result might point to a more serious problem, such as colorectal cancer or other gastrointestinal malignancies. The presence of cancer cells in the digestive tract can lead to bleeding, resulting in a positive stool occult blood test.
Importance of Follow-Up Procedures
A positive stool occult blood test necessitates a thorough follow-up procedure. This involves a detailed patient history, a physical examination, and further diagnostic tests to identify the underlying cause of the bleeding.
- Further Diagnostic Testing: Procedures like colonoscopy, endoscopy, or imaging studies (e.g., CT scans) are often employed to visualize the digestive tract and pinpoint the source of bleeding.
- Referral to Specialists: In cases of suspected malignancy, the patient may require referral to a gastroenterologist or oncologist for further evaluation and management.
False Positives and False Negatives
It’s important to acknowledge the potential for false positive and false negative results in stool occult blood tests. A false positive occurs when the test indicates blood is present, but it’s not. A false negative, conversely, means the test doesn’t detect blood when it’s actually present. These errors can lead to misdiagnosis or delayed treatment.
- False Positives: Certain foods (e.g., red meat, beets) or medications (e.g., aspirin) can cause a false positive result. In addition, recent use of laxatives or enemas can also lead to a false positive result.
- False Negatives: These can occur if the sample is not properly collected or if the bleeding is intermittent or not severe enough to be detected by the test.
Comparison of Benign and Malignant Causes
The following table provides a comparative overview of benign and malignant causes of positive stool occult blood tests. It Artikels the potential symptoms, diagnostic tests, and treatments for each.
Navigating the intricacies of the ICD-10 code for stool occult blood screening under Medicare can be complex. However, understanding these nuances is crucial, especially when considering potential implications stemming from unforeseen circumstances, such as being involved in a car accident with liability insurance, like in this scenario i have liability insurance and was hit by another car.
Ultimately, accurately obtaining the appropriate ICD-10 code remains paramount for proper medical billing and reimbursement.
| Cause | Symptoms | Diagnostic Tests | Treatment |
|---|---|---|---|
| Benign (Hemorrhoids) | Rectal pain, bleeding, itching | Visual examination (anoscopy), physical exam | Lifestyle modifications, topical creams, or surgery in severe cases |
| Benign (Anal Fissures) | Painful bowel movements, bleeding | Visual examination (anoscopy), physical exam | Fiber-rich diet, stool softeners, topical treatments |
| Benign (Inflammatory Bowel Disease) | Abdominal pain, diarrhea, weight loss | Colonoscopy, biopsies | Medications, dietary changes, surgery |
| Malignant (Colorectal Cancer) | Changes in bowel habits, blood in stool, abdominal pain, unexplained weight loss | Colonoscopy with biopsies, imaging studies | Surgery, chemotherapy, radiation therapy |
Documentation and Reporting
Proper documentation and reporting of stool occult blood screening results are crucial for accurate diagnosis and appropriate patient management. This process ensures that Medicare reimbursements are handled correctly, and most importantly, provides a clear record of the patient’s care. Thorough documentation also facilitates communication between healthcare providers and aids in future reference.Accurate documentation ensures that the results of the stool occult blood screening are properly interpreted and used in the patient’s care.
This process is critical for appropriate management of potential gastrointestinal conditions.
Necessary Documentation
Thorough documentation is essential for stool occult blood screening. This includes a detailed patient history, physical examination findings, and the results of the test itself. Patient history should include details about any relevant symptoms, family history of gastrointestinal issues, and current medications. The physical examination should document any abnormalities observed.
Patient History
Patient history is paramount for context. It should detail any relevant symptoms, such as abdominal pain, blood in the stool, changes in bowel habits, or weight loss. Family history of colon cancer or other gastrointestinal disorders should be noted. Current medications, including over-the-counter drugs, should be listed. This information helps in understanding the patient’s overall health status and potential risk factors.
Physical Examination
The physical examination should document any relevant findings. This includes noting any abdominal tenderness, masses, or other abnormalities. Vital signs should also be recorded.
Test Results
The test results are the core of the documentation. Clearly state whether the result is positive or negative. If positive, specify the intensity of the reaction. Any unusual findings, such as a positive result in an area not typically expected to show blood, should be noted. Include the date and time of the test.
Examples of Documentation
Positive Result
Patient presented with complaints of intermittent abdominal pain and dark stools for the past two weeks. Physical exam revealed mild tenderness in the left lower quadrant. Stool occult blood test was positive, with a moderate reaction noted. Further evaluation is recommended.
Negative Result
Patient presented with no complaints of abdominal pain or blood in the stool. Physical exam was unremarkable. Stool occult blood test was negative. No further testing is indicated at this time.
Reporting to Medicare
Medicare requires specific formats for reporting stool occult blood screening results. The format should include the patient’s demographic information, the date of the test, the result (positive or negative), and any relevant clinical findings. Medicare guidelines should be consulted for the exact format and required fields.
Steps for Completing and Submitting Paperwork
- Review the Medicare guidelines for specific reporting requirements.
- Gather all necessary patient information, including demographic data, test results, and any relevant clinical notes.
- Complete the appropriate Medicare claim form, ensuring all required fields are filled out accurately.
- Ensure the form is signed and dated by the appropriate healthcare provider.
- Submit the completed form according to Medicare’s submission guidelines. These may include electronic submission or mail submission.
Patient Education and Counseling
Educating patients about stool occult blood screening is crucial for ensuring accurate results and appropriate follow-up. Clear communication empowers patients to understand the test’s purpose, procedure, and potential outcomes, leading to higher compliance. This section will detail effective strategies for patient education and counseling, including a sample patient handout.
Strategies for Patient Education
Effective patient education involves a multi-faceted approach that goes beyond simply providing information. It includes active listening, addressing concerns, and tailoring explanations to the patient’s comprehension level. Crucially, patients need to understand the rationale behind the test and the implications of the results, positive or negative.
Importance of Patient Counseling
Patient counseling is paramount to address anxieties and concerns about the procedure. Patients may have questions about discomfort, potential side effects, or the implications of a positive result. Empathetic and supportive counseling can alleviate these concerns and foster a sense of trust and cooperation. It also ensures the patient feels comfortable enough to ask questions. This fosters a partnership between the healthcare provider and the patient, maximizing the effectiveness of the screening process.
Sample Patient Education Handout
This handout provides a concise overview of the stool occult blood screening process and potential implications of the results. It should be written in clear, simple language, avoiding medical jargon.
- Introduction: Briefly explain the purpose of the test and its importance in early detection of colorectal cancer. Emphasize that it’s a routine screening test for individuals at average risk.
- Procedure: Detail the steps involved in collecting the stool sample. Include instructions on sample preparation and handling, ensuring the sample reaches the lab in optimal condition. Provide clear instructions on the timing of sample collection relative to meals and medications.
- Potential Results: Explain both positive and negative results, highlighting the meaning of each. Positive results indicate the presence of blood in the stool, which may or may not require further investigation. Negative results are reassuring but don’t eliminate the need for further screening in the future, especially for individuals with risk factors.
- Next Steps: Artikel the anticipated follow-up procedures for both positive and negative results. Positive results may necessitate further tests like colonoscopies. Negative results might mean a return to routine screening in the future, depending on individual risk factors.
- Questions and Contact Information: Provide space for patients to ask questions and a contact number or email address for further clarification.
Importance of Clear Communication
Clear communication is vital to ensure patient understanding and compliance. Use plain language, avoid medical jargon, and actively encourage questions. Provide visual aids, if appropriate, to enhance understanding. Active listening is crucial to ascertain the patient’s level of comprehension and address any misunderstandings.
Quality Assurance and Control
Stool occult blood screening, while a valuable tool, relies heavily on meticulous quality control. Accurate results are crucial for patient management, and deviations from established protocols can lead to misdiagnosis and inappropriate treatment. This section details the procedures for ensuring accuracy and reliability in this screening process.
Procedures for Quality Assurance
Maintaining the accuracy and reliability of stool occult blood screening tests requires a multifaceted approach. Rigorous adherence to established protocols for sample handling, analysis, and reporting is paramount. This includes standardized procedures for specimen collection, transport, and storage, as well as strict adherence to manufacturer’s instructions for the chosen test method. Internal quality control measures, along with external proficiency testing, are vital components of a robust quality assurance program.
Monitoring Test Accuracy and Reliability
Several methods are employed to monitor the accuracy and reliability of stool occult blood screening tests. Positive and negative controls are routinely included in each batch of tests to validate the performance of the test reagents and equipment. The percentage of correctly identified positive and negative results, alongside the calculation of the sensitivity and specificity of the test, are key indicators of the test’s performance.
Regular review of these metrics allows for prompt identification of any trends or deviations from expected values. For instance, a consistent decrease in sensitivity might indicate reagent degradation, necessitating replacement.
Adherence to Established Protocols
Adherence to established protocols is critical to ensure the quality and validity of stool occult blood screening results. Proper handling of specimens from collection to analysis, adhering to temperature guidelines, and meticulously documenting each step are essential. Deviation from these protocols can lead to false-positive or false-negative results, impacting patient care. For example, inadequate refrigeration of samples can compromise the integrity of the test, potentially affecting the outcome.
Each laboratory must establish and document a detailed protocol manual, readily accessible to all personnel involved in the process.
Potential Sources of Error and Corrective Actions
Several factors can contribute to errors in stool occult blood screening. Improper specimen collection techniques, inadequate storage, and equipment malfunctions are potential sources of error. Careful record-keeping and systematic investigation of errors are essential for identifying the root cause and implementing corrective actions. For instance, if a high rate of false-positive results is observed, the laboratory should investigate factors such as reagent expiration dates, instrument calibration, and operator training.
Implementation of corrective actions is critical to restoring test accuracy and reliability.
Quality Control Measures
| Quality Control Measure | Frequency | Expected Outcome |
|---|---|---|
| Positive and Negative Controls | Each test batch | Positive controls should consistently yield a positive result; negative controls should consistently yield a negative result. |
| Internal Proficiency Testing | Weekly/Monthly | Maintain acceptable levels of sensitivity and specificity for the test method. |
| External Proficiency Testing | Quarterly/Annually | Compare laboratory performance to other laboratories using the same test method. |
| Reagent Verification | Before each batch | Verify that reagents are within the specified expiration dates and appropriate storage conditions. |
| Equipment Calibration | Daily/Weekly | Ensure instruments are calibrated according to manufacturer specifications. |
Regulatory Considerations
Stool occult blood screening, while a valuable diagnostic tool, is subject to a variety of regulations and standards. Understanding these regulations is crucial for healthcare providers to ensure accurate testing, proper patient care, and compliance with legal requirements. Compliance ensures patient safety and protects healthcare organizations from potential penalties.Ensuring compliance with regulatory frameworks is essential to maintain quality, reliability, and patient safety in the context of stool occult blood screening.
These standards dictate various aspects, from the testing process itself to the reporting and documentation of results. Non-compliance can lead to serious repercussions, including financial penalties, legal challenges, and reputational damage.
Relevant Regulations and Standards
Numerous regulatory bodies and standards oversee the practice of stool occult blood screening. These organizations establish guidelines to maintain the accuracy, reliability, and safety of the screening process. The standards define acceptable testing methodologies, quality control procedures, and reporting requirements.
Compliance Requirements
Adherence to compliance requirements is paramount. This encompasses a range of activities, including using validated test kits, following established protocols for sample collection and handling, implementing quality control measures, and correctly interpreting and reporting results. Failure to adhere to these requirements can compromise the validity of test results and potentially impact patient care.
Examples of Compliance Standards
Several examples illustrate the impact of compliance standards. One example involves the use of validated test kits, which are rigorously tested to ensure accuracy and reliability. Another critical example relates to standardized procedures for sample collection and handling. Proper handling protocols prevent contamination and ensure the integrity of the sample, thereby maintaining the accuracy of the results.
These protocols are meticulously designed to maintain the integrity of the results.
Table of Regulatory Bodies, Standards, and Compliance Requirements
| Regulatory Body | Relevant Standards | Associated Compliance Requirements |
|---|---|---|
| Clinical Laboratory Improvement Amendments (CLIA) | CLIA ’88 | Certification and accreditation for laboratory proficiency; strict quality control procedures; established testing methodologies; and personnel training. |
| Centers for Medicare & Medicaid Services (CMS) | Medicare guidelines for reimbursement | Appropriate documentation of test procedures and results; accurate coding; adherence to billing guidelines; and provision of patient education materials. |
| College of American Pathologists (CAP) | CAP accreditation standards | Use of validated test kits; adherence to standardized testing procedures; and implementation of quality control measures. |
| Food and Drug Administration (FDA) | FDA-approved test kits | Use of FDA-cleared or approved test kits; adherence to manufacturer’s instructions for use; and proper disposal of materials. |
Final Conclusion
In conclusion, this discussion on ICD-10 codes for stool occult blood screening under Medicare highlights the intricate interplay between clinical practice, coding procedures, and reimbursement policies. Accurate documentation and understanding of Medicare coverage criteria are paramount for efficient and compliant billing. By following the guidelines Artikeld in this document, healthcare providers can effectively navigate the complexities of this process and ensure optimal patient care.
Answers to Common Questions
What are some common causes of a positive stool occult blood test result?
Possible causes range from benign conditions like hemorrhoids and anal fissures to more serious issues such as colorectal cancer. Further investigation is crucial to determine the precise cause.
How long does the stool occult blood screening typically take to process?
Typical turnaround times for stool occult blood screening tests vary depending on the laboratory and the specific testing method used. The table in the introduction section provides further detail on typical turnaround times.
What documentation is needed for Medicare reimbursement?
Accurate and complete documentation, including patient history, physical examination findings, and test results, is essential for successful Medicare reimbursement. Section 5 of the Artikel provides more detailed information.
Are there any potential errors in stool occult blood screening?
False positives and false negatives can occur. Factors like diet, medications, and other underlying conditions can influence results. Section 4 of the Artikel details these potential sources of error and their implications.
